Sick Bay News

Doctors in Secondary Schools
A Victorian Department of Education and Training partnership.
The Doctors in Secondary Schools program provides primary health care services to 100 Victorian Government secondary schools. The program funds a general practitioner (GP) and Practice Nurse (PN) to provide onsite primary care for students up to one day per week.
Fit-for-purpose clinic consultation facilities have been installed onsite at all participating schools as part of the program. The initiative complements existing student wellbeing programs aimed at improving health literacy, and preventive health.
The Program is funded by the Victorian Department of Education and Training (DET) and implemented by Victoria’s six Primary Health Networks (PHNs). PHNs are supporting the GPs to be integrated with community-based primary care services to enable best-practice, patient-centred care.
Objectives
The objectives of the program are:
- make primary health care more accessible to students.
- provide assistance to young people to identify and address any health problems early; and,
- aim to reduce the pressure on working parents and community-based GPs.
All GPs, PNs and school staff are provided with training in adolescent health, at no cost. School-based GPs bulk-bill consultations through Medicare and are remunerated for time spent that cannot be billed. There are no out-of-pocket expenses for students who attend consultations with participating GPs and PNs.
Craigieburn Secondary College is part of this initiative. The Doctor is at school every Friday for any consultation that our students may require. Appointments can be made via telephone, or in person by students, at the school Sick Bay.
As a general overview, here are a few health checks that are important for teenagers:
- Blood pressure check.
- Dental check-up.
- Growth check.
- Mental health check.
- Skin check.
- Reproductive health check.
- Fatigue.
- Sleep issues.
- Wound management.
- Routine blood tests (for example iron issues).
- And plenty more…
Medical Action Plans
Your child’s health and safety is extremely important to us. Therefore, we need to know about any medical conditions your child has. Medical conditions, such as Anaphylaxis, Allergies, Asthma and Eczema can be very serious and may require emergency treatment at school. It is important that we have up to date information about the management of your child’s condition and this needs to be updated every 12 months.
To help us provide the best medical care for your child, we request that you complete an Action Plan. Action Plans can be collected from the office or downloaded from our website. The Action Plan must be completed in consultation with your family doctor and should be returned to us as soon as possible – or we can arrange an appointment with the Doctor’s in School program and get this done for you. This ensures we have up to date medical information for your child for the start of each school year. If there is no standard Action Plan available for your child’s condition, please provide written information from a health care professional detailing appropriate treatment.
You can access copies of plans to be completed by copying the appropriate link below:
Allergic Reactions Action Plan
Anaphylaxis Plan
- https://www.allergy.org.au/hp/anaphylaxis/ascia-action-plan-for-anaphylaxis
The school can provide hard copies of each of these if you require – please contact the Sick Bay for assistance.
Melbourne’s Hay Fever Season: How to Cope
Hay fever season in Melbourne runs from the 1st of October to the 31st of December each year. It is a period dreaded by the 4.5 million Australians who suffer from the condition. Itchy ears and throat, a runny nose, sneezing, and watery eyes can all impact your day.
- What is hay fever?
- How long does hay fever last?
- What’s the best cure for hay fever?
- Melbourne’s pollen count
- Thunderstorm asthma
- When to visit your GP
- About Dr Elaine Sung
For an unfortunate few, the effects of hay fever are much more severe. Headaches, tiredness and difficulty concentrating can make springtime unbearable. Grass pollen in the air is a significant cause of hay fever, and pollen levels are the highest in late spring and early summer. The good news is pollen counts are published daily during hay fever season, allowing people affected by the condition to take precautions.
What is Hay Fever?
Also known as allergic rhinitis, hay fever is an allergic reaction to airborne particles, particularly pollen. In Melbourne, ryegrass pollens are usually to blame. These pollens get trapped in the tiny hairs inside your nose, often triggering an allergic reaction. Your immune system thinks it’s under attack. Nasal cavities become inflamed, causing your body to create more mucus. This is in an attempt to flush out the irritating particles.
The high levels of airborne pollen seem ruthless from late spring to early summer. It can feel like you are getting hit from all directions, with no end in sight. Luckily, some people fare better than others and escape the worst of the season.
How Long Does Hay Fever Last?
Hay fever lasts as long as there is sufficient pollen and other allergens are in the air to cause an allergic reaction. Once Melbourne’s hay fever season finishes, usually by January, most people find their symptoms disappear.
In saying this, many people experience episodes throughout the year. Dust mites, mould and household pets are also common irritants.
On a day-to-day basis, hay fever can last anywhere from a couple of hours to days. This duration depends on many factors, including your sensitivity to specific airborne allergens and how you minimise your exposure. The common cold, which lasts for a few days to a week, is sometimes mistaken for hay fever. However, symptoms such as aches and pains, fatigue, and a mild fever tell you it is more likely a cold.
What’s the Best Cure for Hay Fever?
We cannot cure hay fever. Allergen immunotherapy is the best treatment for people with severe symptoms or those who do not respond to medications. Also known as desensitisation, immunotherapy exposes your immune system to gradual concentrations of the offending allergen. Courses of treatment can run over several months, with treatment continuing for a few years. The treatment involves a doctor administering allergen molecules through injections, tablets or drops placed under your tongue. For the rest of us, there is a range of over-the-counter medications to help reduce hay fever symptoms. These include:
- steroid nasal sprays (e.g. Rhinocort Hayfever, Nasonex and Telnase)
- antihistamines (e.g. Zyrtec and Claratyne)
- eye drops (e.g. Visine-A and Naphcon-A)
- decongestants (e.g. Otrivin and Dimetapp)
Your GP (or the Doctor’s in School Program) can also advise what prescription medications may suit you.
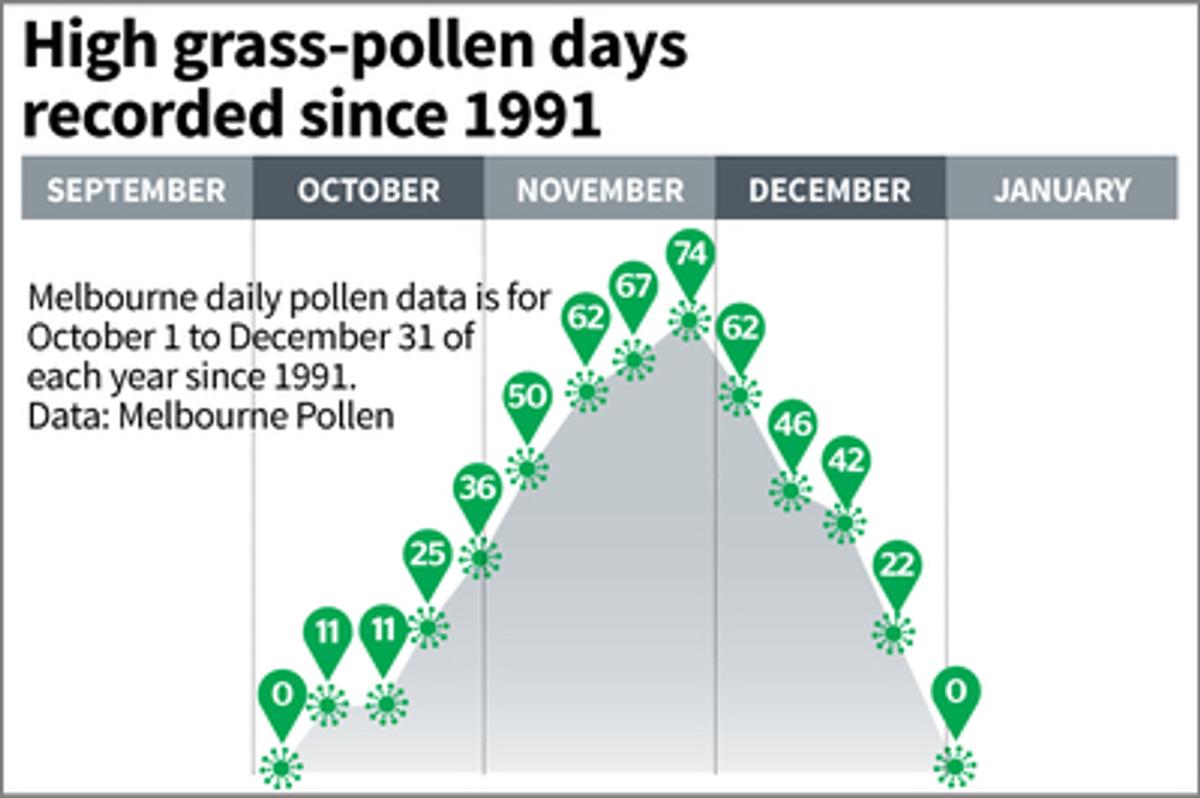
Melbourne’s Pollen Count
Melbourne’s daily pollen count is active from October to January, with peak readings towards the end of November. We urge hay fever sufferers to know the daily pollen forecast and stay indoors during high pollen days. A high-pollen day is when there are 50 or more pollen grains per square metre of air, and extreme days see more than 100 grains per square metre. Two essential tools for preparing for these high-risk days are the Melbourne Pollen Count app and the VicEmergency app. Both apps provide forecasts for thunderstorm asthma events and give you access to many other helpful features.
Thunderstorm Asthma
Melbourne is known globally as a notorious site for thunderstorm asthma.
You may remember the shocking thunderstorm asthma event in late November 2016. Nine people died, and many more were hospitalised. It was an unprecedented incident that led us to take preventative measures. People with hay fever have an increased risk of asthma, including during a thunderstorm asthma event. Many victims of the 2016 event had no previous asthma symptoms.
A thunderstorm asthma event can happen when a high or extreme pollen day combines with a particular type of storm. A sudden change in humidity causes pollen to burst into tiny particles. This turbocharges the spread of pollens, magnifying their terrifying effects.
The University of Melbourne’s School of BioSciences has an excellent FAQ which you can refer to for further information.
When Visit Your GP (or the Doctor’s in School Program can assist)
You probably know what to do on bad days if you have had hay fever for a while.
However, I recommend you get to your GP if any of the following happens:
- You experience asthma symptoms such as a cough that will not stop, breathlessness, wheezing or chest tightness
- Your hay fever symptoms last a week or more
- Your usual over-the-counter hay fever medications are not working
- You experience side effects from these medications.
Your GP can also refer you to a specialist if you want an allergy test. Some people find allergy testing useful in determining the exact trigger of their hay fever.