Sick Bay News

Let’s talk Asthma….
Let’s talk Hay Fever….
Let’s talk about the Doctor at the school program…
What is Asthma?
Asthma is a serious and long-term condition that affects 1 in 9 Australians. Sadly, more than 400 Australians die of asthma each year. There is currently no cure, but in most cases asthma can be well managed and people with asthma can live a full life.
Having asthma means you have sensitive airways. Your airways can become inflamed or swollen when you are exposed to your triggers. There are 3 changes that can happen in your airways when triggered:
- Your airway walls become thicker from swelling.
- Your airways fill up with mucous.
- Your airways feel tight from the muscles on the outside of the airways squeezing.
These changes in your airways make it hard to breathe. You may feel like you are breathing through a very thin tube.
How Will I Know If I have Asthma?
Your doctor can tell you if you have asthma. Keep in mind that we have a doctor at the school every Friday that can help with this. Just book an appointment through the sick bay (this is all via Medicare). Getting a diagnosis of asthma means that your doctor will need to talk to you about your medical history. This will include your symptoms, when you get symptoms and how you treat them. Your doctor might also ask you to have a lung function test such as spirometry. Asthma affects people of all ages and is common in both kids and adults. It is not something you can grow out of, and just because you do not currently have any symptoms does not mean that it is gone. You can be diagnosed with asthma for the first time at any age or stage of life.
Understand your asthma with the Asthma Control Questionnaire (ACQ5)
Asthma can be a frustrating and unpredictable condition. It can make it difficult to breathe, exercise, and sleep. One simple tool for managing asthma is the Asthma Control Questionnaire. It is a recognised clinical asthma symptom measurement tool in Australia and internationally.
Start the Asthma Control Questionnaire
Why should you take the Asthma Control Questionnaire?
This is a simple, quick, 5 – question survey that can help you assess how well your asthma is under control. It helps you understand your asthma symptoms and track your progress over time. If you find out your asthma is not under control, you can talk to your doctor about it. They will work with you to find the right treatment for you.
Who can complete the Questionnaire?
The Asthma Control Questionnaire is suitable for anyone with asthma aged 12 years and older. For kids aged 7 to 11 years, it is better for parents or carers to contact our Asthma Educators to complete the questionnaire together.
What happens when you complete the questionnaire?
Once you submit your answers to the Asthma Control Questionnaire, you will be prompted to provide some basic details. This is so we can send you a copy of your responses, your results and recommended next steps.
Asthma Educators Can Answer Your Asthma Questions
Book a FREE phone call at a time that works for you or call direct on 1800ASTHMA (1800 278 462).
“An Asthma Educator really changed my life. I have never in my life been more well than I am now, due to that call I made to Asthma Australia. Can’t recommend them highly enough. I learned more in that 40-minute chat than I have in my lifetime.” 1800 ASTHMA Caller
Please note:1800 ASTHMA service is only available for people residing in Australia
1. Book a call with an Asthma Educator at a time convenient to you using the form below
2. Email asthmasupport@asthma.org.au
3. Call 1800 ASTHMA (1800 278 462) between 9am-5pm AEST Monday-Friday and PRESS 1 to talk to an Asthma Educator about -
- Asthma in children
- How to care for someone with asthma
- What to do after you have been to hospital for your asthma
- Hay fever/allergic rhinitis and your asthma
- Severe asthma
- Colds and flu and your asthma
- What to ask your pharmacist or doctor
- Asthma and pregnancy
- Asthma and smoking
- Australian best-practice asthma management
- Asthma diagnosis
- Asthma medicines and how to use them
- Asthma devices and how to use them
- Spacers
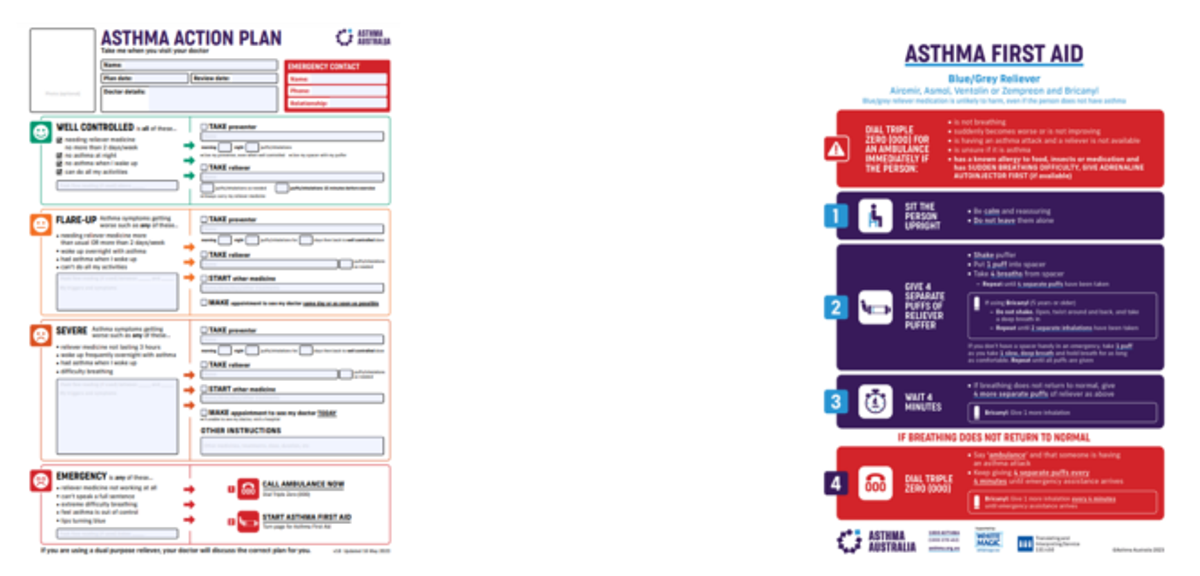
- Asthma Action Plans
- Asthma First Aid
- Triggers and what sets off your asthma
- Asthma symptoms
Do you need an Interpreter or National Relay Service?
Asthma Australia welcomes calls through the National Relay Service. If you are deaf, have a hearing impairment and/or have a speech impairment you can choose your access option information here and provide our phone number 1800 278 462 when asked by the Relay Officer.
For more information, visit the NRS website communications.gov.au/accesshub/nrs to choose your preferred access point or call the NRS Helpdesk on 1800 555 660. If English is not your first language, you can still call the Translating and Interpreting Service (TIS National) on 131 450 and ask them to telephone the Asthma Australia on 1800 278 462.
What are the symptoms of asthma?
Not all people with asthma have the same symptoms. Not all people with asthma have all the symptoms. Asthma symptoms are the signs, effects or feelings that you may notice as a result of having asthma. Your asthma symptoms are caused by changes in the airways (breathing tubes) of your lungs. These changes make it harder to breathe.
The most common asthma symptoms are:
1. Cough
A cough happens because your airways have narrowed, and more mucus has formed. A cough caused by asthma might be:
- an on-going cough or one that won’t go away
- a cough that only occurs during the night or early morning
- a cough during sport or activity
- a cough when excited or laughing.
2. Wheezing
A whistling or squeaky sound when you breathe is made by the narrowing of your airways
3. Shortness of breath
Feeling breathless, or out of breath, because your airways are too narrow to allow the air you need in or out.
4. Chest tightness
This might feel like something is squeezing or sitting on your chest. This is the feeling of the muscles around your airways tightening. Symptoms range from mild to more serious. Asthma symptoms are often worse at night or early morning, making it hard to sleep. You might have other symptoms that include:
- feeling tired
- increased heart rate
- becoming sweaty.
These symptoms may happen because of the extra work needed for breathing. Using all your chest muscles to help with your breathing means you need more energy, which makes your heart beat faster. We also know that:
- symptoms can be different from person to person
- symptoms can change for one person from one time to another
- symptoms can be every now and then, or all the time.
What Are Silent Symptoms?
Some people with asthma may have silent symptoms. They may not notice any asthma symptoms until they become really unwell. Being breathless can be a silent symptom. It is not as obvious to you or others as coughing a lot or wheezing. It can also be ignored or passed off as being unfit or tired. For people with silent symptoms, sometimes their doctor will ask them to use a peak flow meter to help them measure whether their airways are narrowing. If you or someone you care for has silent asthma symptoms, you should let people around you (doctors, school/daycare staff, work colleagues, family and friends) know so they can help and support you when you need it.
Symptoms In Kids
Asthma symptoms in kids can be harder to spot. Kids have much smaller breathing tubes (airways) than adults. This means even small changes to how their airways work can make a big difference to their breathing.
As kids cannot always tell us their symptoms, we need to rely on all our senses to understand what might be happening. Knowing what symptoms to look for can help you and your doctor decide on the right course of action for your child. Like adults, they may not have all the symptoms, but some things to look out for include:
1. Being breathless or difficulty breathing
Think about how your child breathes when they are well. This makes it easier to look for symptoms when they are unwell. For all kids, especially our younger ones, look for these signs and symptoms of breathing difficulty or being breathless:
- Does your child breathe through their mouth or their nose?
- If they have a virus or a blocked nose from allergies, breathing through their nose is more difficult. When their nose cannot filter, warm or moisten the air they breathe, breathing in air through their mouth may irritate their small breathing tubes.
- Changes in how your child breathes:
- Look at their body while they breathe. Are they breathing faster than usual or are there any sounds made while breathing?
- Are they using their body to help them breathe? For example, raising their shoulder when they take a breath.
- Activity levels:
- Does your child get out of breath while playing or stay out of breath for longer than usual?
- Is your child avoiding activities because they get breathless?
- Are they quieter or more irritable than usual?
- Have they said they have a sore tummy?
More serious signs that your child is struggling to breathe and needs emergency help include:
- the soft area at the bottom of their throat (where it meets the chest) is sucking in and out during breathing
- their tummy is sucking in or pumping up and down
- the muscles between the ribs are sucking in when they take a breath
- their lips are turning blue.
- they are unable to finish their sentences or eat because they are so breathless
Any sign of breathing difficulty should result in a visit to the doctor. These symptoms will help your doctor to understand your child’s condition and decide which treatment will be best for them. It is important to tell them about all your child’s symptoms, even if you feel like they are normal.
2. Wheezing
A wheeze is a high-pitched whistling sound made by the airways when they are narrowing. It can sometimes be easy to hear, or your doctor may hear it as they listen to your child’s breathing using a stethoscope. A wheeze can be caused by several things, including asthma. However, not all children will have a wheeze with asthma.
A wheeze is more likely to be asthma if it is:
- very frequent
- worse at night or early in the morning
- happens when your child does not have a cold
- occurs in reaction to a trigger.
Talk to your doctor if your child has a wheeze.
3. Coughing
Coughs in kids can be caused by many things, and there are lots of different types of coughs. Sometimes coughing brings up mucus or phlegm. No matter how the cough sounds, talk to your doctor if your child has:
- an ongoing cough or one that will not go away
- a cough that only occurs during the night or early morning
- a cough during sport or activity
- a cough when excited or laughing.
4. Chest Tightness
Kids might feel chest tightness when the airways are so narrow it is difficult to get the air in or out. This might make them feel like there is a heavy weight on their chest. Your child might say things like “I’m feeling sick” or “I have a sore tummy”. If your child or a child you care for is experiencing this symptom it is important to see a doctor and review their symptoms or seek a diagnosis.
How To Manage Symptoms
We want people with asthma to live free from their symptoms. How you take care of your symptoms will affect how well your asthma is managed.
The first step in managing your asthma is knowing:
- what your symptoms are
- how to treat your symptoms
- how to avoid triggering your symptoms.
Knowing how bad or how often you get asthma symptoms will help you and your doctor to better understand how to treat them. A written Asthma Action Plan from your doctor will also help you to organise this information all in one place. To keep track of your symptoms, you can use an app such as Kiss My Asthma or use the Calendar or Notes app on your phone to record them. A good tip is to assign the symptoms to different calendar colours. You can also create a simple table on a page or use sticky notes to track your symptoms. You can record your symptoms over several days or a couple of weeks before visiting your doctor.
Are You Getting Used To Asthma Symptoms?
Sometimes, you or your child might have asthma symptoms so often that you get used to these symptoms. It becomes the ‘new normal’ way of being or breathing. Ignoring
or putting up with symptoms can be dangerous because your asthma can become worse more quickly. Without treatment of your symptoms, there may also be long-term damage to your lungs. If you have trouble with your symptoms, talk with your doctor about how they can help.
What Should I Do If I Think I Have Asthma Symptoms?
If you suspect you or your child might have asthma after reading about the symptoms, you should see your doctor for a diagnosis. Do not ignore the symptoms – if you or your child do have asthma, the sooner you get it under control, the faster you can get back to living a full and active life. Use Asthma First Aid to treat worsening symptoms that are not improving.
Asthma Educators can answer your asthma questions
Book a FREE phone call at a time that works for you or call us direct on 1800ASTHMA (1800 278 462).
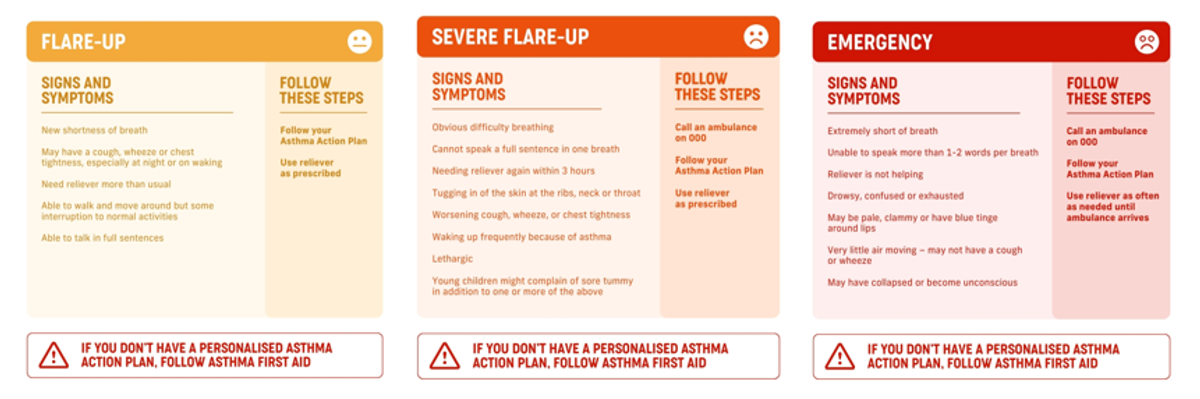
WHAT IS AN ASTHMA FLARE-UP?
An asthma flare-up can also be called an ‘asthma attack’ or ‘exacerbation’.
Asthma symptoms might begin to flare up or get worse slowly (over hours or days). This kind of flare-up may begin with mild symptoms but can become severe. Or asthma symptoms might become severe very quickly (in seconds to minutes). This kind of flare-up is what most people know as an asthma attack. Depending on how bad the symptoms are, this could also be called a ‘severe’ or even ‘life-threatening’ flare-up.
WHAT IS A BAD ASTHMA FLARE-UP?
Asthma symptoms and flare–ups come in all shapes and sizes. An asthma flare-up might look or sound different for different people. The most common symptoms of an asthma flare-up are worsening cough, persistent wheeze, being short of breath and feeling tight in the chest. During a flare-up you might feel like your reliever is not working or does not work for as long as usual.
HOW DANGEROUS CAN ASTHMA GET?
All asthma flare-ups are bad, but some flare-ups are more life-threatening than others.
Around 400 people a year die from a severe asthma flare-up in Australia. Repeat flare-ups, over time, are linked to faster loss in lung function. This table helps you check how serious an asthma flare-up might be.
How close are you to a flare–up? Do the Asthma Control Questionnaire (ACQ5) to find out how controlled your asthma is this week.
WHAT IS A ‘SILENT’ ASTHMA ATTACK?
Not all people with asthma will have a wheeze or cough during an asthma flare–up. But they may still have other severe or life-threatening symptoms. In fact, for many, once an asthma flare–up reaches an emergency level, their cough or wheeze disappears. This is because their airways have squeezed so tight that they can no longer get enough air in and out to make those sounds. This is very dangerous.
WHAT IS THE AFTERMATH OF AN ASTHMA ATTACK?
An asthma flare-up can be very scary. Maybe you were able to treat it yourself, or maybe you had to go to hospital. If you were prescribed rescue tablets or liquids for your child (oral corticosteroids) you might feel some side-effects over the next few days. If you or
your child has had an asthma flare-up or attack, even with mild symptoms, book a visit to your doctor to review your asthma care to recover, and make plans to do all you can to prevent another flare-up. This might include starting, changing or increasing your preventer. Preventers are key for preventing asthma flare-ups, avoiding the need for rescue tablets or liquids, and keeping healthy lungs. To help get back on track after your visit to the emergency department or hospital, click below to visit our after-hospital page.
Hay Fever Season Has Arrived (allergic rhinitis)
Key facts
- Hay fever (allergic rhinitis) is an allergic response from your immune system that causes sneezing, runny nose and watery, itchy eyes.
- Hay fever can be triggered by seasonal allergens like pollens and grass or year-round triggers like dust mites, and animal fur.
- See your doctor if your hay fever symptoms are ongoing and affect your day-to-day living.
- Most people manage hay fever by avoiding allergens in their daily life, and with medicines such as antihistamines and nasal sprays.
- Allergy testing can help to identify potential triggers for hay fever but should be considered together with your history and other symptoms.
On this page
- What is hay fever?
- What are the symptoms of hay fever?
- What causes hay fever?
- When should I see my doctor?
- How is hay fever diagnosed?
- How is hay fever treated?
- What are the complications of hay fever?
- Resources and support
- Other languages
- Related information on Australian websites
What is Hay Fever?
Hay fever is the common name for allergic rhinitis. Hay fever describes a reaction that occurs when your nose or eyes come in contact with allergens, which are substances to which you are sensitive. Allergens can include pollens, dust mites, moulds, animal dander, or other substances. For some people, exposure to these allergens can trigger an immune response (your body’s natural defence system), which leads to swelling and inflammation in the inner lining of the nose (known as rhinitis). Hay fever is common — it affects 1 in
5 people in Australia. Despite its name, it is not caused by hay and does not cause a fever.
What are the symptoms of hay fever? Common symptoms include:
- an itchy, runny or blocked nose
- itchy or watery eyes
- frequent sneezing
- needing to breathe from your mouth
- frequently needing to clear your throat
- feeling like you have a cold that will not go away
- snoring during sleep
Less common symptoms of hay fever may include:
- interrupted sleep, that may lead to feeling tired during the day
- difficulty concentrating
- frequent headaches and/or facial pain
- recurring sore throats
- a reduced sense of smell
- frequent sinus infections in adults
- recurring ear infections (otitis) in children
You might only experience some of these symptoms, and still have hay fever or allergic rhinitis. Some of these symptoms can be caused by other diseases too.
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes hay fever?
Common allergens that may trigger hay fever symptoms include:
- grass, weeds and tree pollens
- dust mites and dust
- animal fur or skin flakes
- moulds and fungal spores
- air pollutants
- latex
You may experience hay fever symptoms only at certain times of the year (such as in spring or summer), depending on the allergens to which you are sensitive. Hay fever and other allergies can also be affected by your genes. You may have the same or different triggers to your family members. Most people are able to manage or relieve hay fever on their own. However, you should speak with your doctor about treatment options if your symptoms are:
- persistent — meaning that you experience symptoms at least 4 days in a week, for at least 4 weeks or more
- moderate to severe — meaning that your symptoms affect your sleep and daily activities such as work, school, sport and leisure
Your doctor can help you by asking you in detail about your symptoms. They will review your home and work environment for possible triggers, assess how intense your hay fever symptoms are and how much hay fever affects your day-to-day life. They can then organise further tests to investigate possible causes and help you find ways to manage or avoid hay fever in the future. If your symptoms are mild or occasional, you can ask your pharmacist for advice.
How is Hay Fever Diagnosed? History, your doctor can diagnose hay fever from a description of your symptoms and when they occur. They may also ask what over the counter or prescribed medicines you already take for hay fever. It is also a good idea to record and tell your doctor about any triggers you have noticed in your work or home environment, and how hay fever affects your quality of life. Physical examination,
to rule out other causes of your symptoms, your doctor may:
- examine your face (especially your nose and eyes) for signs of hay fever
- ask you to breathe through your nose
- examine your nostrils with a special scope (a tiny camera attached to a long, thin tube)
- examine your throat
Allergy testing, Allergy testing (for example, using a blood test or skin prick test) is the main way to learn whether your hay fever symptoms are caused by a particular allergen. You may be referred to a clinical immunologist or allergy clinic for this test. If you have skin prick testing, a tiny amount of a suspected allergen will be dropped onto your skin (usually on the forearm, upper arm or back). The doctor or nurse doing the test will then prick your skin where the allergen was placed. If you are allergic to this specific allergen, the place where you were pricked will become swollen and itchy. This generally goes away within 2 hours. Although skin prick testing can be uncomfortable, most people find it tolerable. The results are available within 20 minutes.
Any allergy testing needs to be considered alongside your history and symptoms of hay fever. A positive test result does not prove that the allergen is causing your symptoms, only that your body is sensitive to the allergen. Taking too many allergy tests may sometimes cause confusion and cause you unnecessary lifestyle changes to avoid many types of allergens that may not actually be causing your symptoms. Speak with your doctor about what the results of your allergy test mean, and whether you need to make changes to your lifestyle.
How is hay fever treated? Hay fever can be treated in 4 main ways, depending on what you are allergic to and how severe your symptoms are:
Minimise Exposure to Allergens
If you know which allergens trigger your hay fever, reducing your exposure to them may reduce symptoms. If pollens are causing your hay fever, these tips may help:
- Stay indoors until after midday, especially when the pollen count is high, it is windy or after thunderstorms (you can check today’s pollen count at the Pollen Forecast Network website).
- Wear sunglasses, carry tissues, shower when you arrive home and rinse your eyes with water.
- If your trigger is grass, avoid mowing, playing or walking in grassy areas and do not go camping on grass.
- Keep your windows closed at home and in the car and use recirculating air conditioning in the car.
- Avoid outdoor picnics during pollen season.
- Try to plan holidays out of the pollen season, or holiday at the seaside.
- If you are gardening at home, research which plants are less likely to trigger hay fever. Remove any weeds or vegetation outside your bedroom window that might trigger symptoms.
Nasal Irrigation
For some people, saltwater nasal sprays or douches (a stream of water sprayed into the nose) will provide substantial relief from hay fever. These non-medicated approaches are safe and can often help relieve symptoms.
Medicines
While medicines cannot cure hay fever, they can reduce your symptoms effectively.
Their side effects are generally well tolerated. Ask your doctor or pharmacist about the following medicines:
- Intranasal corticosteroids: These are nasal sprays that effectively reduce inflammation in the lining of the nose caused by hay fever or other conditions. Corticosteroid nasal sprays must be used regularly and correctly to be effective. Different brands are available, so ask your doctor which one is right for you. Ask your pharmacist how to use your nasal spray, to be sure you are using it correctly.
- Antihistamines: These medicines manage symptoms of hay fever by blocking the action of histamine, which the body releases in response to exposure to an allergen. In this way, antihistamines reduce the symptoms of the allergic reaction. They are available as tablets, syrups, nasal sprays and eye drops to offer localised relief where you are experiencing hay fever symptoms. For example, use eye drops for itchy or watery eyes.
- Combination medicines: These contain an antihistamine and an intranasal corticosteroid. They offer the advantages of both medicines.
- Decongestant sprays: These unblock and dry the nose, but they should not be used for more than a few days at a time. This is because they can cause problems such as 'rebound congestion'. This is when your symptoms become worse after you stop using the decongestant.
- Decongestant tablets: These also unblock and dry the nose, but they can have stimulant side effects such as tremors, difficulty sleeping, anxiety or increased blood pressure. Speak with your pharmacist to check if decongestant tablets are suitable for you, especially if you have high blood pressure.
Immunotherapy
Allergen-specific immunotherapy, also known as ‘desensitisation’, is a therapy designed to reduce the intensity of the body’s reaction to an allergen. Immunotherapy works by gradually exposing someone to increasing doses of allergen extracts, either by injection or orally. This is a long-term treatment option and should only be started by a medical specialist such as a clinical immunologist. What are the complications of hay fever?
Complications of hay fever may include:
Hay fever may also trigger frequent ear infections, such as otitis media in children, and sinus infections (sinusitis) in adults. Untreated hay fever may also increase the risk of developing asthma or make asthma harder to control, so it is especially important to treat your nasal symptoms if you have asthma. This is because asthma and hay fever are both associated with airway inflammation. About 4 in every 5 people with asthma also have hay fever.
Resources and support
For more information and support, try these resources:
- Download the AirRater app to track your hay fever symptoms and monitor allergens in the environment.
- Check the pollen count at PollenForecast, to find the pollen count for your area.
- Asthma Australia explains how hay fever can make asthma worse.
Other languages
Do you prefer other languages than English? The National Asthma Council has translated its Asthma & Allergy factsheets into Arabic, Chinese and Vietnamese.
Remember we have a doctor that comes to the school every Friday for the students – appointments can be made through the sick bay and this is covered under Medicare.
The Doctors in Secondary Schools Program (DiSS) funds general practitioners (GPs) and practice nurses to attend 100 Victorian Government secondary schools up to one day a week to provide medical advice and health care to those students most in need. Craigieburn Secondary College has this facility – the doctor is local to the community and works from the Hanson Road Medical Centre in Craigieburn. We can organise blood tests, scripts, referrals, x-rays, scans and more.