Health News: Sick Bay

Head Knocks/Injuries
It is policy that when any head knock, injury or strike occurs, the school will call parents to notify them. This must be done even if there is no acute injury.
The assessment process that occurs in the sick bay is as follow:
- Student is assessed if they can fully recall the incident
- Their conscious state is assessed
- They are asked if they feel nauseous
- They are asked if they have a headache
- They are asked if they fell after getting hit
- If there is any altered sensation felt in their arms and legs
- If there was any visual disturbance after the head strike
- If there is any swelling, bruising or redness where the strike happened
- Assess if the student is unsteady on their feet
- They are checked for cervical tenderness
So, any head strike/injury/knock is thoroughly assessed when the student presents to sick bay and please remember that parents will be notified of any incident as per policy, even if there is no actual acute injury.
Assessment when a student presents to sick bay
If a student attends the sick bay for any reason they are assessed to see if they are acutely unwell. This involves the following:
- Heart rate
- Respiratory rate
- Conscious state
- Temperature
- Chest auscultation
- Blood pressure
- SPO2 levels
- Pain score
- Blood glucose levels (with parents’ approval)
- Type of injury/Illness
- When it happened/started
- Type of pain felt
- Urinary & bowel movements
- Any signs of dehydration
- Oral intake with food & fluid
Processes and plans are made if the student is not acutely unwell.
Please remember that there is a doctor that attends to the school every Friday and is available for any appointment that a student may require.
The objectives of the program are to:
- make primary health care more accessible to students
- assist young people to identify and address any health problems early
- reduce the pressure on working parents.
Please use the QR code below for more information regarding this great program available at Craigieburn Secondary College.
Please use the QR code for further information regarding consent and confidentiality relating to the Doctors in Secondary School Program.
Vaccination Program for secondary students at Craigieburn Secondary College
Students in years 7, 8 and 10 can receive free vaccinations at school through the National Immunisation Program.
These free vaccinations include:
- human papillomavirus (HPV) vaccine – offered in year 7 or 8, depending on your state or territory
- diphtheria-tetanus-pertussis (dTpa) vaccine – offered in year 7 or 8, depending on your state or territory
- meningococcal ACWY vaccine – offered to Year 10 students
Trained and qualified vaccination teams visit schools to deliver the vaccines throughout the year.
To make sure your child is vaccinated…The school will provide a vaccination consent form. Year 7’s have already been vaccinated on the 13th of May, and Year 10’s consent forms are coming soon. The child’s parent or guardian must sign the form and return it to the school before the child can be vaccinated.
As a parent or carer, it’s important to talk to your child about the importance of immunisation. If you need help to start the conversation and get them prepared, watch our vaccination videos for high school students.
If your child misses a vaccination at school, see your GP or other immunisation provider to catch-up on the vaccination they missed.
Information regarding vaccination will be sent out soon via Compass and a hard copy sent home with each student. In the meantime, please follow the instructions below to register beforehand.
The Year 10 vaccination date is the 13th of July. In Year 10, students require one immunisation: meningococcal A,C,W,Y vaccine (one dose).
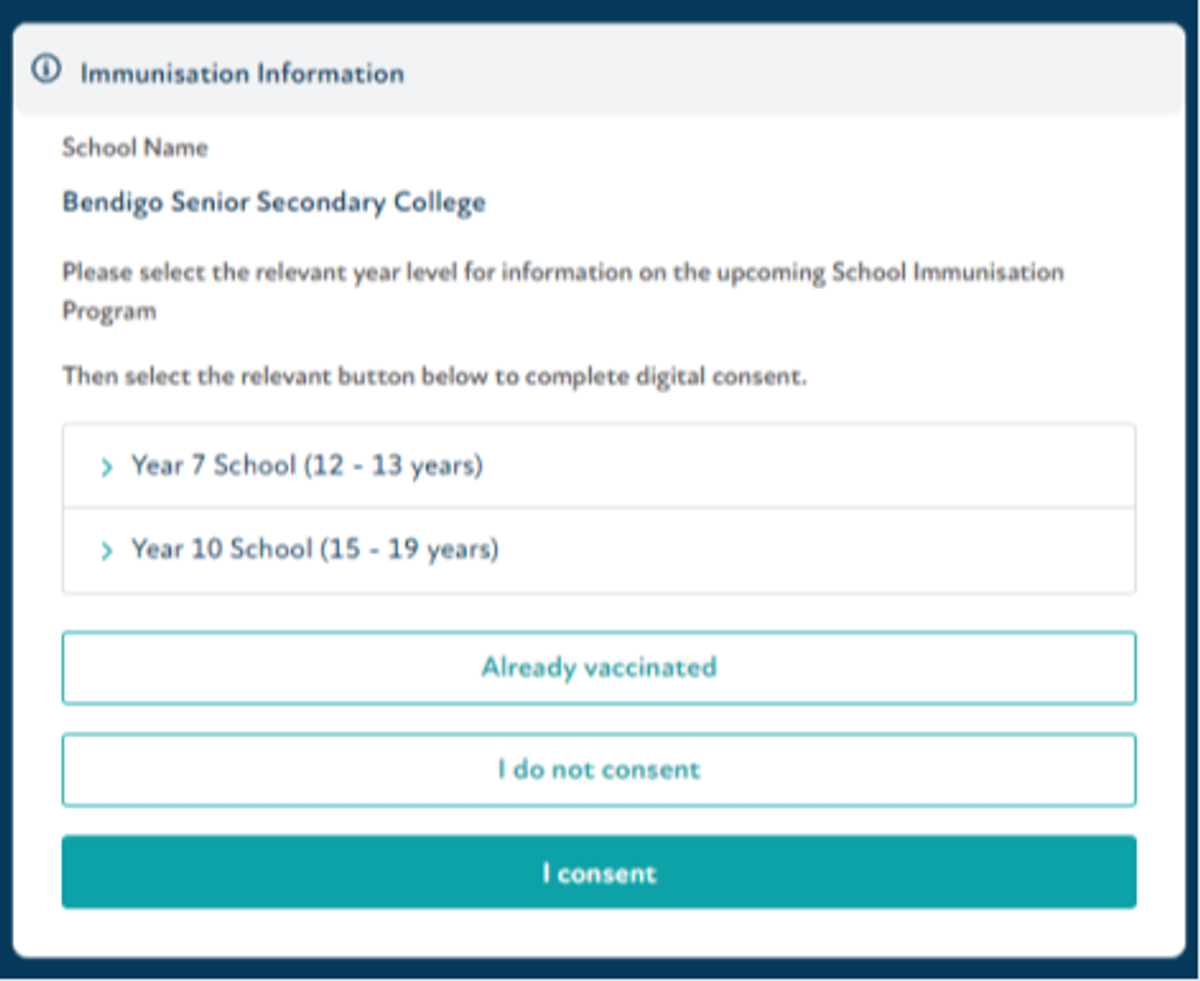
Hume City Council will provide these immunisations through your child’s school, Craigieburn Secondary College. Consent for these vaccines is submitted through VaxApp, an immunisation platform used by Hume City Council. To get started you need to provide consent for immunisations.
Please use the link provided below or the QR code:
https://hume.book.vaxapp.com.au/school/CraigieburnSecondaryCollege-AywrcR
You will be shown three consent options:
1. ‘I consent’ – you wish for your child to be immunised
2. ‘Already vaccinated’ – your child has already received these vaccines elsewhere
3. ‘I do not consent’ – you do not wish for your child to be immunised
When you click ‘I consent’ you will need to create a profile for yourself and then your child. If you have multiple children attending the same school for Immunisations, you will need to do this separately for each child. If you are consenting for multiple children, you will only need to make one profile for yourself, and your details will appear for each child. You will need to re-click the link for each child you are consenting for, and you will need to fill out certain details for each student, but these are minimal.
It is important that you register and submit a response, regardless of which option you choose. This will prevent you from receiving additional follow-up calls or messages.
If you do not wish your child to be immunised at school, free immunisation is provided at any of Hume City Council’s immunisation sessions. These sessions are via appointment only. You can book an appointment online via www.hume.vic.gov.au\immunisation If you have any questions regarding the immunisation program, please contact the Immunisation Department on 9356 6745.
Smile Squad is the Victorian government's free school dental program
Smile Squad delivers free oral health promotion, dental check-ups and treatment to Victorian government school students. Good oral health prevents dental problems before they become serious. Smile Squad helps students stay engaged in school and ready to learn.
This program is being led by the Department of Health and Dental Health Services Victoria, with input from the Department of Education. Services are currently being delivered across Victoria by local community dental agencies. The program is completely free for all Victorian government school students. Students will be seen by the Smile Squad during school hours, saving families time and money. Smile Squad includes all required treatment (excluding orthodontics).
Objectives of Smile Squad
- Students can receive free dental care regularly
- Students learn about the importance of good dental care
- Students will have better oral health outcomes through early intervention.
Regular dental checks can prevent or address dental health issues before they become serious.
What to expect?
Dental packs and oral health promotion are provided to all students. Dental check-ups are carried out in school classrooms using portable equipment and further treatment is delivered in our treatment vans that house a full dental clinic. Think of it as a dental clinic on wheels.
Your friendly Smile Squad staff include oral health therapists, dental therapists, oral health educators, dental assistants, dentists, and specialists
A registration form with be handed out to each student as the Dental Van will be visiting the school in the week of the 28th of October. The registration form will need to be returned to school by the 31st of July.
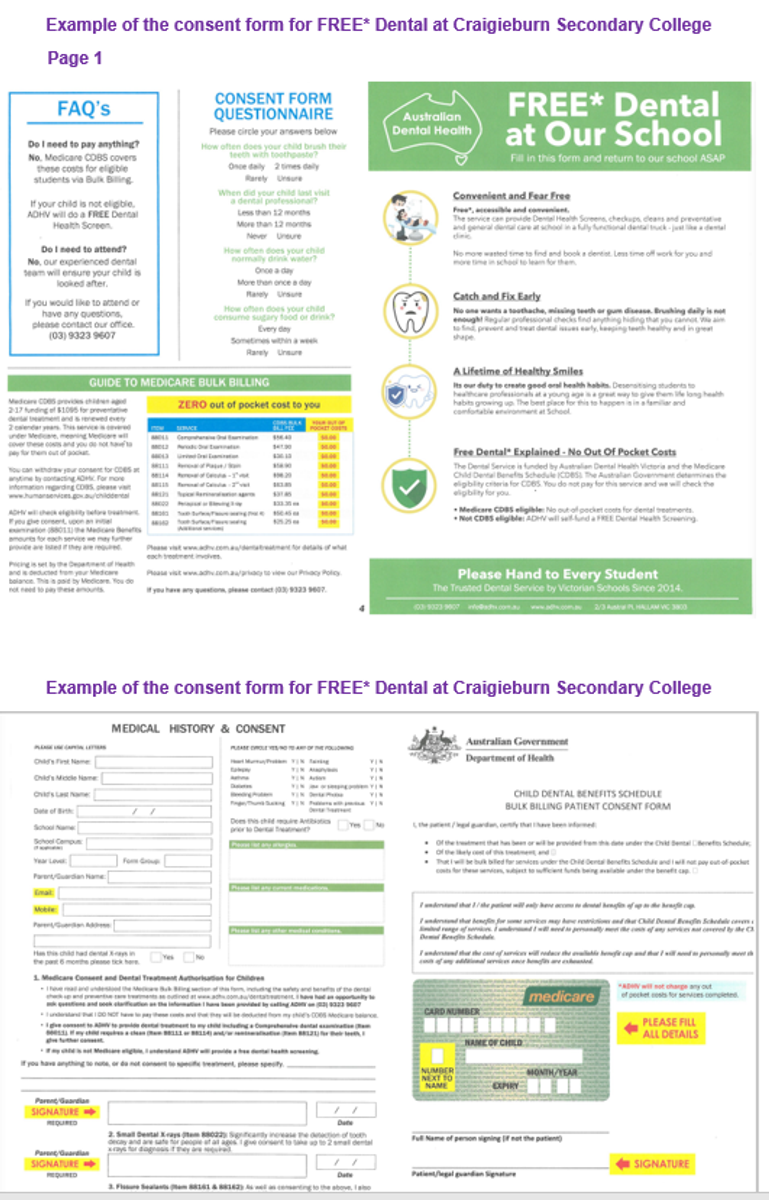
Example of the consent form for FREE* dental at Craigieburn Secondary College
National Immunisation Program
2024 Influenza (Flu) Vaccination
Consumer fact sheet
About influenza
Influenza is a common viral infection that affects people of all ages. While it may be a mild disease for some, it can also cause serious illness and even lead to hospitalisation in otherwise healthy people. Vaccination, administered annually by a health professional is the safest means of protection from influenza.
About the influenza vaccines
The strains of the virus circulating can change yearly, prompting updates to the vaccines based on expert advice. That’s why it is important to get vaccinated every year.
The vaccine brand used will depend on age. Your health professional can tell you which vaccine they will use for you or your child’s immunisation.
All National Immunisation Program funded vaccines available for use in 2024 are quadrivalent, covering four strains.
Egg based vaccines and a cell-based vaccine (for people aged 5 - 64 years) are available on the program. There is no preferential recommendation for either. They are all latex free.
Influenza vaccine safety
The influenza vaccine has been around for many decades and has a great safety record.
Common side effects from the vaccine include mild pain, redness or swelling where the vaccine was given. These side effects usually last for a few days and go away without any treatment.
Serious side effects, such as a severe allergic reaction are rare. The vaccine does not contain live influenza viruses and cannot cause influenza. People with an egg allergy, including history of anaphylaxis can safely receive all influenza vaccines. If you have an egg allergy, please discuss this with your health professional.
Who should receive the influenza vaccine? Everyone 6 months and over is recommended to get an influenza (flu) vaccine each year. The flu vaccine protects you, but it also can help protect those around you.
Children under 5 years
Babies and children younger than 5 years have a higher risk of complications from influenza potentially leading to hospitalisation. Even healthy children can get very sick from influenza.
Your child can get an influenza vaccine either on its own or at the same appointment as their other routine childhood vaccinations.
Children under 9 getting the influenza vaccine for the first time need 2 doses, 4 weeks apart. This strengthens the immune response to all vaccine strains.
Pregnant women
Influenza is a serious disease for pregnant women and their babies. The influenza vaccine is recommended and free for every pregnancy. It’s safe to give at any stage during pregnancy. It’s safe while breastfeeding.
Changes to immune, heart and lung functions during pregnancy increase vulnerability to severe influenza related complication.
Vaccination in pregnancy enables the transfer of protective antibodies to the baby through the placenta. This protects them in their vulnerable early months when they are too young to be vaccinated themselves.
Pregnant women who had last year’s influenza vaccine early in their pregnancy are recommended to have the current influenza vaccine before the baby is born.
If you received the vaccine before pregnancy, you should be revaccinated during pregnancy to protect your unborn infant.
Influenza vaccination can safely be given at the same time as pertussis, COVID-19, or other vaccines recommended during pregnancy.
People with certain medical conditions
The influenza vaccine is free for people 6 months and over with the following conditions:
- cardiac disease
- chronic respiratory condition
- immunocompromising condition
- haematological disorder
- chronic metabolic disorder
- chronic kidney disease
- chronic neurological condition
- long-term aspirin therapy in children aged 5 to 10 years.
Talk to your health professional about your medical history and eligibility.
Aboriginal and Torres Strait Islander People
Aboriginal and Torres Strait Islander people are at higher risk of getting really sick and going to hospital from influenza. All Aboriginal and Torres Strait Islander people aged 6 months and over can get the influenza vaccine for free every year.
People aged 65 years and over
Vaccination is very important for people aged 65 years and over as they are at high risk of getting sick from influenza. All adults aged 65 and over are eligible for a free influenza vaccine that is specifically made to boost the immune response for better protection.
When to get your influenza vaccine
You should get vaccinated each year from April onwards to be protected before the influenza season. The peak influenza season is usually June to September in most parts of Australia. However, it is never too late to get the vaccine as influenza can spread all year round. If you had last season’s flu vaccine late last year or early this year, you should still get the new season vaccine this year when it becomes available.
Australian Immunisation Register
Your health professional is required to report all influenza vaccinations to the Australian Immunisation Register, ensuring accurate records.
Ask about the flu vaccine today health.gov.au/flu
| State and territory health department contact numbers: | |
| ACT 02 5124 9800 | SA 1300 232 272 |
| NSW 1300 066 055 | TAS 1800 671 738 |
| NT 08 8922 8044 | VIC immunisation@health.vic.gov.au |
| WA 08 9321 1312 | QLD Contact your local Public Health Unit |
Important – please read!!!
There have been several students that we have found recently with low iron levels, so please read the following information and if you think it is necessary, we can then make an appointment for bloods tests with the doctor that attends the school every Friday.
What is iron?
Iron is an important mineral involved in various bodily functions, including the transport of oxygen in the blood. This is essential for providing energy for daily life. Good sources of iron include red meat, offal and iron-fortified breakfast cereals. Iron is lost from the body through sweat, shedding intestinal cells, and blood loss. About one third of the world’s population is iron deficient. Menstruating women are at greater risk than men and postmenopausal women of iron deficiency. It is thought that up to 5% of the Australian population has iron deficiency anaemia.
Roles of iron in the body
Some of the many roles of iron in the body include:
- Oxygen transport – red blood cells contain haemoglobin, a complex protein that carries oxygen from the lungs to the rest of the body. Haemoglobin is partly made from iron, and accounts for about two thirds of the body’s iron.
- Myoglobin – a special protein that helps store oxygen in muscle cells. Myoglobin contains iron and is responsible for the red colour of muscle.
- Enzymes – many enzymes throughout the body contain iron, including those involved in energy production. Enzymes are catalysts (they increase the rate of chemical reaction) that drive many cell functions.
- Immune system– proper functioning of the immune system relies, in part, on sufficient iron. The immune system helps us fight infection.
Recommended dietary iron intake
The average person needs to absorb just a small amount of iron each day to stay healthy (around 1 mg for adult males and 1.5 mg for menstruating females). To achieve this, however, we need to consume several times that amount. This is because our bodies absorb only a fraction of the iron contained in the foods we eat. The Australian Recommended Dietary Intake (RDI) for iron is the amount of dietary iron required to meet the needs of most of the population. This amount is different depending on factors like age groups and life stages.
Food sources of iron
The 2 types of iron found in our diets are:
- Haem iron – found in animal tissue such as beef, lamb, kangaroo, chicken and fish. Offal products such as liver and kidney are particularly rich in haem iron (however pregnant women should avoid eating too much offal as it contains large amounts of vitamin A, which can cause birth defects). This form of iron is most easily absorbed by the body.
- Non-haem iron – found in animal tissue, animal-based products and plant foods such as dried beans and lentils. Good vegetarian sources of non-haem iron include iron-fortified breakfast cereals, wholegrains and legumes (beans and lentils). If you are vegetarian and have no animal tissue in your diet, you may need almost twice as much dietary iron each day as non-vegetarians. Plant-based sources of iron include: dark green leafy vegetables such as broccoli, raisins, nuts, prunes, dried apricots, seeds, dried beans and peas, and iron-fortified cereals, breads and pastas.
Absorbing iron our diet
How much iron you absorb from your diet depends on how much iron your body is storing.
The healthy body absorbs around 18% of the available iron from a typical western diet (which includes animal foods) and about 10% from a vegetarian diet. However, you may be absorbing much less than that, even if your diet includes iron-rich foods.
The most significant influence on iron absorption is the amount of iron already stored in your body. The body stores iron in various places, including the liver. If your stores are high, your body absorbs less iron from the foods you eat. Conversely, low iron stores increase your ability to absorb iron.
Dietary factors affecting iron absorption
Certain foods and drinks affect how much iron your body absorbs.
To boost iron absorption:
- Consume vitamin C (found in fruits and vegetables).
- Include animal protein (haem) with plant (non-haem) sources of iron, such as meat with beans – for example, beef and kidney beans in a chilli con carne.
- Cook plant sources of iron (such as vegetables). In most cases, cooking increases the amount of available non-haem iron in vegetables. For example, the body absorbs 6% of the iron from raw broccoli, compared to 30% from cooked broccoli.
Foods and drinks that reduce your body’s ability to absorb iron:
- Soy proteins can reduce absorption from plant sources.
- Tea, coffee and wine contain tannins that reduce iron absorption by binding to the iron and carrying it out of the body.
- Phytates and fibres found in wholegrains such as bran can reduce the absorption of iron and other minerals.
- Inadequate vitamin A in your diet could lead to iron deficiency because vitamin A helps to release stored iron.
- Calcium and phosphorus reduce the absorption of plant-sourced (non-haem) iron.
High-risk groups for iron deficiency
One in 8 people aged 2 years and over do not consume enough iron, on average, to meet their needs. If you do not have enough iron in your body, it is called being ‘iron deficient’. This can make you feel tired and lower your immunity. Including iron-rich foods in your diet can help.
People who are at an increased risk of iron deficiency, include:
- babies given cow’s or other milk instead of breastmilk or infant formula
- toddlers, particularly if they drink too much cow’s milk
- teenage girls
- menstruating women, especially those who have heavy periods
- women using an IUD (because they generally have heavier periods)
- pregnant women
- breastfeeding women
- people with poor diets such as people who are alcohol dependent, people who follow ‘fad diets’, or people with eating disorders
- people who follow a vegetarian or vegan diet
- Aboriginal Australians
- athletes in training
- people with intestinal worms
- regular blood donors
- people with conditions that predispose them to bleeding, such as gum disease or stomach ulcers, polyps or cancers of the bowel
- people with chronic diseases such as cancer, autoimmune diseases, heart failure or renal (kidney) disease
- people taking aspirin as a regular medication
- people who have a lower than normal ability to absorb or use iron, such as someone with coeliac disease.
Stages and symptoms of iron deficiency
Most of your body’s iron is in the haemoglobin of your red blood cells, which carry oxygen to your body. Extra iron is stored in your liver and then used by your body when your dietary intake is too low. If you don’t have enough iron in your diet, your body’s iron stores get lower over time. This can cause:
- Iron depletion – when haemoglobin levels are normal, but your body only has a small amount of stored iron, which will soon run out. This stage usually has no obvious symptoms.
- Iron deficiency – when your stored and blood-borne iron levels are low and your haemoglobin levels have dropped below normal. You may experience some symptoms, including tiredness.
- Iron deficiency anaemia – when your haemoglobin levels are so low that your blood is unable to deliver enough oxygen to your cells. Symptoms include looking very pale, breathlessness, dizziness and fatigue. People with iron deficiency anaemia may also have reduced immune function, so they are more vulnerable to infection. In children, iron deficiency anaemia can affect growth and brain development.
Symptoms of iron deficiency anaemia in children
The signs and symptoms of iron deficiency anaemia in children may include:
- behavioural problems
- repeat infections
- loss of appetite
- lethargy
- breathlessness
- increased sweating
- strange ‘food’ cravings (pica) like eating dirt
- failure to grow at the expected rate.
Causes of iron deficiency in adults
In adults, some of the common causes of iron deficiency include:
- Not getting enough iron in your diet (also known as ‘inadequate dietary intake’). There are many reasons why someone’s dietary intake of iron could be too low, for example due to a poorly balanced vegetarian diet, chronic fad dieting or having limited access to a wide range of fresh foods.
- Blood loss – iron deficiency easily occurs in situations of chronic (ongoing) blood loss. Common causes include heavy menstrual periods, regular blood donation, regular nosebleeds, other chronic conditions that involve bleeding (such as peptic ulcers, polyps or cancers in the large intestine), and certain medications, particularly aspirin.
- Increased need for iron – if you are pregnant or breastfeeding your body needs more iron. If this increased need isn’t met, iron deficiency can quickly occur.
- Exercise – athletes are prone to iron deficiency because regular exercise increases the body’s need for iron in several ways. For example, hard training promotes red blood cell production (which requires iron), and iron is lost through sweating.
- Inability to absorb iron – healthy adults absorb about 10 to 15% of dietary iron, but some people’s bodies are unable to absorb or use iron from food.
Causes of iron deficiency in babies, children and young people
Major risk factors for the development of iron deficiency in children include:
- prematurity and low birth weight
- exclusive breastfeeding beyond 6 months (not introducing solids)
- high intake of cow’s milk in young children less than 2 years of age
- low or no meat intake
- vegetarian and vegan eating
- poor diet in the second year of life
- possible gastrointestinal diseases
- lead poisoning.
Babies, children and teenagers undergo rapid growth spurts, which increase their need for iron. The main causes of iron deficiency in children by age group include:
- Babies less than 6 months old – newborns receive their iron stores in the uterus (womb), which means the mother’s diet during pregnancy is very important. Low birth weight or premature babies are at increased risk of iron deficiency and will need iron supplements (under medical supervision only). See your doctor for further advice.
- Babies aged 6 months to one year – a baby’s iron stores run low in the second half of their first year. Iron deficiency can result if their diet doesn’t include enough iron-rich solid food. At around 6 months, 2 servings a day of plain, iron-fortified infant cereal mixed with breastmilk or infant formula can start to be given. Plain pureed meats can soon be offered with other solids, once your baby is used to the cereal. Late introduction of solids into the baby’s diet is a common cause of iron deficiency in this age group.
- Children aged one to 5 years – breastmilk contains a small amount of iron, but prolonged breastfeeding can lead to iron deficiency, especially if breastmilk replaces solid foods in the diet. Low-iron milks such as cow’s milk, goat’s milk and soymilk should not be given until 12 months of age. Children who drink milk in preference to eating solid foods are in danger of iron deficiency.
- Teenagers – adolescent girls are at risk because of several factors, including growth spurts at puberty, iron loss through periods (menstruation) and risk of under-nutrition due to fad dieting that restricts eating.
- In general – gastrointestinal disorders, such as coeliac disease, are a rare but possible cause of anaemia in children.
Preventing iron deficiency in teenagers
To prevent iron deficiency in teenagers:
- Talk to your child about the importance of iron. Help them become informed enough to make their own responsible food choices.
- Encourage iron-rich foods and meals, such as iron-fortified breakfast cereals and breads, and serve meat, poultry or fish with the evening meal.
- Offer good sources of non-haem iron such as dried beans, lentils, peas, broccoli, spinach, beans, fortified cereals, breads and whole grains if your child wants to avoid red meat or become vegetarian. Vitamin C-rich foods should also be encouraged, such as fruits or vegetables with meals.
- Encourage only moderate amounts of tea and coffee, as these can interfere with iron absorption.
Diagnosing iron deficiency
Make an appointment with your doctor if you think you may be iron deficient. Diagnosis aims to exclude other illnesses that can have similar symptoms, such as coeliac disease.
Diagnosis methods include:
- physical examination
- medical history
- blood tests – the doctor that attends the school every Friday can do blood tests.
Treatment for iron deficiency
Treatment for iron deficiency depends on your iron status, and the underlying cause:
- If you have iron depletion, your doctor will give you information about including iron-rich foods in your diet. You will have another blood test in around 6 months to check that your iron level has improved.
- If you have iron deficiency, your doctor will give you dietary advice and closely monitor your diet. They will encourage you to have iron-rich foods and discourage you from having foods and drinks (such as bran, tea and coffee) that can interfere with iron absorption with meals. They will regularly review your iron status and may prescribe supplements.
- If you have iron deficiency anaemia, your doctor will prescribe iron supplements. It may take between six months and one year for your body to restock its iron stores. Your iron levels will be regularly reviewed with blood tests.
- If you have an underlying problem that is causing your iron deficiency, it is very important that the cause is investigated. If it is a medical cause, it is important that it be treated appropriately.