Food Gut Microbiome and Depression:

A new study takes an important step forward in understanding the relationship of gut bacteria to what we eat and how we feel.
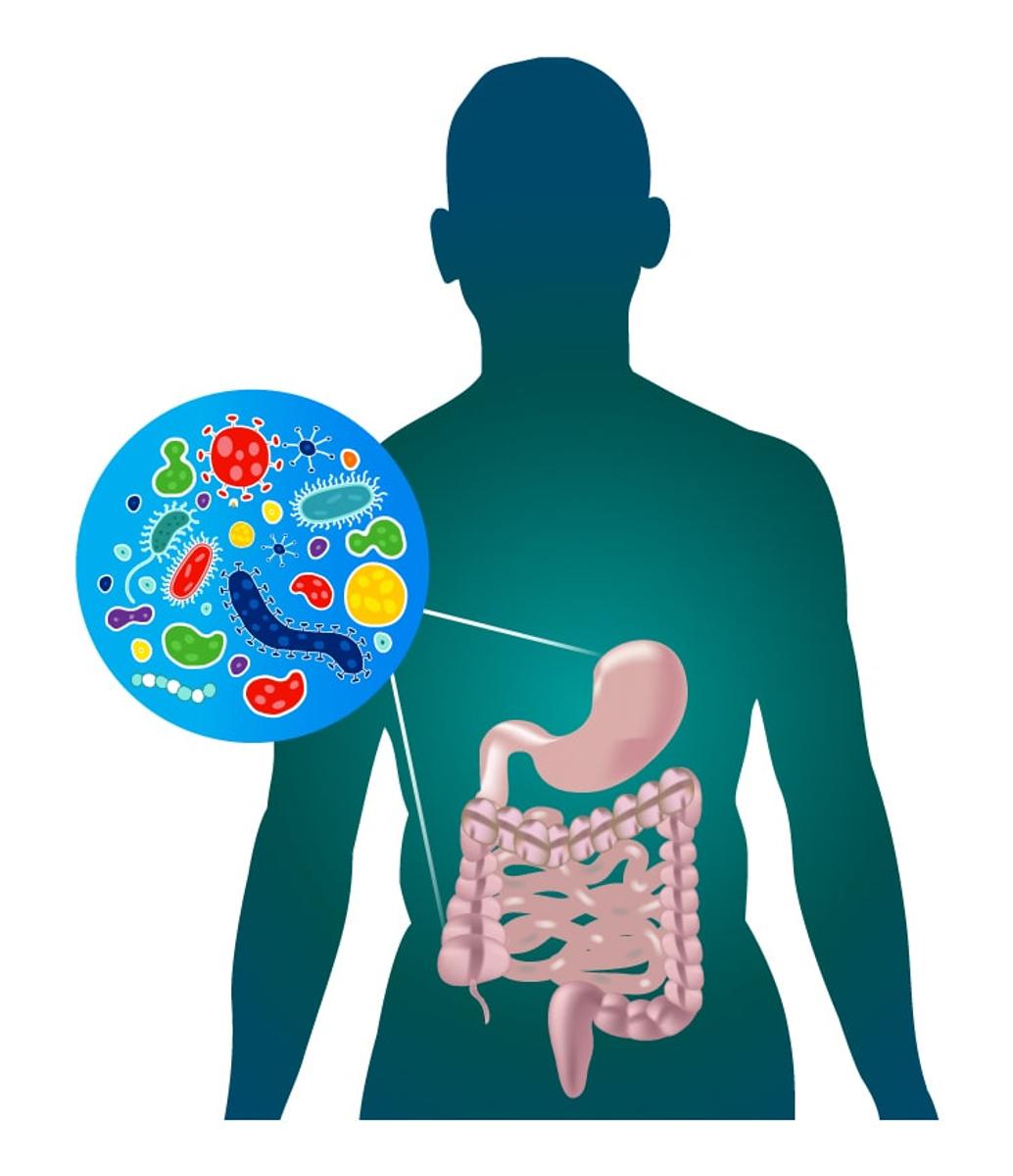
Research has long suggested a link between our diet and our mental health. The gut microbiome — the collective genome of trillions of bacteria that live in the intestinal tract that are created largely by what we eat and drink — appears to influence our mood and mindset.
The most extensive analysis of depression and the gut microbiome to date, published in December, found several types of bacteria notably increased or decreased in people with symptoms of depression.
“This study provides some real-life evidence that you are what you eat,” says study author Andre Uitterlinden, who researches genetics at Erasmus Medical Centre in Rotterdam, Netherlands.
Or, to be exact, how you feel is closely related to what you consume.
The gut-brain axis
Interest in the gut-brain axis has had a resurgence in the past 20 years. A host of studies has pointed to a connection between the microbiota living in our intestinal tract, and our minds, including our memory, mood and cognitive skills.
Such research has spawned an industry of probiotics, prebiotics and fermented everything. Scientific names like bacteroidetes and lactobacillus, two of the most common bacteria found in healthy humans, have become household terms.
In one noteworthy study, entitled “Transferring the Blues,” bacteria-free rats given fecal samples from humans diagnosed with major depression became anxious and disinterested in pleasurable activities. Their metabolism of tryptophan, a chemical connected to depression, changed.
Changing your diet to improve your mood
This is where diet enters the picture. An individual who does not consume enough fibre, for example, may experience a decrease in butyrate-producing bacteria, leading to stress and inflammation and, potentially, symptoms of depression.
It may feel like a letdown that the message from all this work is to eat plenty of fruits and vegetables and not so much sugar. But the sheer amount of research confirming the power of a healthy gut has become undeniable.
The evidence points to the fact that eating healthy, exercising and taking mindfulness breaks can have big benefits.
Research is slowly illuminating exactly how bacteria talk to the brain. For example, many of them produce short-chain fatty acids such as butyrate and acetate, which influence brain activity. Others generate a chemical called GABA, deficits of which are linked to depression.
This progress means that diet may not be the only way to improve our gut colonies. The use of probiotics to prevent and treat depression could become more of an exact science, eventually leading to effective alternatives to antidepressants, and profiling the bacteria could help identify people at risk for depression.
All this research has convinced many researchers that adopting a gut-improving diet comes with just one significant side effect. You’ll get happier.